In 1895, German mechanical engineer physicist Wilhelm Roentgen was experimenting with cathode rays and called his wife Anna Bertha into a darkened room and asked her to put her hand on a black cardboard screen painted with barium platinocyanide placed close to a small aluminum screen.
When she saw her bones, she exclaimed: “I have seen my death!” No live person before had ever seen his own skeleton. X was the mathematical designation for something unknown – but this very first picture using x-rays has changed modern medicine.
Since then, other imaging technologies have joined x-rays – ultrasound, computerized tomography (CT), magnetic resonance imaging (MRI), functional MRI (fMRI) and nuclear medicine imaging, including positron-emission tomography (PET). All these are used to see inside ourselves for diagnosis and treatment without surgery and other invasive procedures.
The endless possibilities of using imaging technologies in medical practice were discussed recently at the 15th Shishi Bari (“Healthy Friday”) lecture series open free to the public by Jerusalem’s Shaare Zedek Medical Center (SZMC).
About 400 people crowded into the hospital’s auditorium to hear and see the latest developments in medical imaging from the medical center’s leading experts, who were presented by Shishi Bari coordinator Dr. Hagit Meskin, chief of pediatric oncology and hematology. None of the hospital’s department are able to function without imaging, she said. Radiologists, x-ray technicians, nurses and others work round the clock and behind the scenes to make this technology possible.
Hospital director-general Prof Jonathan Halevy said that despite the advances in medical robotics, he was not worried that robots would take the place of physicians for imaging. “My doctor son is concluding his studies in medical imaging; I don’t think he will be put out of a job by a robot. We are all people, and we need interaction. Even if, in a decade, there is a computer program that can read and decipher x-ray images, we will always need the human touch to mediate between patient and images and deal with rare and complicated ones.”
Dr. Ofer Benjaminof, head of SZMC’s imaging institute, noted that in 1905, a US hospital was the first to use x-rays during an operation. In 1948 was the first medical use of ultrasound to find stones in the kidneys and spleen; the technology based on sound waves was utilized, after the sinking of the Titanic, to detect glaciers under the surface of the ocean. In recent years, not only static images of the inside of the body were available but also moving images.
Today, doctors have small ultrasound devices that they hold in their pockets and use at the patient’s bedside. A Doppler ultrasound can be used to study blood flow for a variety of medical problems; if there are many blood vessels, said Benjaminof, it may indicate a tumor. Contrast media were injected or swallowed to see movement in the gastrointestinal system and difficulty swallowing. Biopsies can be performed with ultrasound after making only a small incision in the skin to determine whether a patient suffers from liver cancer.
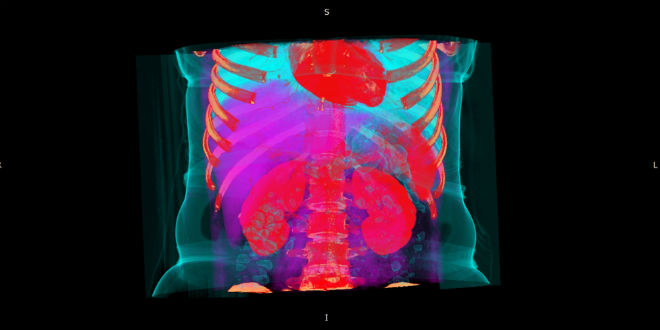
CT scans of the whole body “cut” it into thin slices like a loaf of broad to see details of tissues and organs and then put them together to survey the body from head to toe, said the imaging institute head. The amount of radiation used has been greatly minimized in the most advanced scanners.
The physics for seeing molecules in a magnetic field has been known since the 1950s. The human body is composed mostly of water. Water molecules (H2O) contain hydrogen nuclei (protons), which become aligned in a magnetic field. An MRI scanner applies a very strong magnetic field, which aligns the proton “spins.”
Changes in movement causes energy that is translated into images that can determine if a prostate tumor is growing, if a patient suffers from cirrhosis of the liver, if a child suffers from severe inflammation of the bone and so on. “The technology is getting better all the time,” concluded Benjaminof, whose institute has 110 staffers and who produce 250,000 images a year.
Dr. Naama Bogat, head of the hospital’s heart and chest imaging unit, noted that getting images of the heart is challenging because it is always moving. But with the best technology, one an see calcification inside tiny blood vessels, examine supportive stents in the heart to see if they have narrowed, if a cardiac bypass has clogged up, view inflammation of the heart muscle and even identify tumors in the heart. “Various conditions seem similar, but you can see the differences among them using MRI.”
Dr. Anthony Verstandig performs minimally invasive angiographies as head of the angiography unit. “We use very little radiation to see blood vessels. When they are clogged, we use a tiny balloon to open them and insert a metallic stent to hole the cardiac vessel open. We can also close blood vessels that bleed with stent grafts and open intestines that were clogged. We can treat primary or secondary cancer in the liver and stop bleeding from intestinal ulcers. We can treat varicocele, in which blood vessels swell around the testicle; this condition causes infertility in men. We perform this on 250 patients a year, and many of the wives get pregnant soon after. We also use catheters to remove foreign objects from the body,” said Verstandig.
Dr. Eliel Ben-David, a neuroradiologist and head of the unit for brain and spinal cord imaging, is busy with a wide variety of cases, from strokes and orthopedic problems to cancer, pain and problems with the eyes, mouth and jaw. There are two main types of strokes. The more common – ischemic stroke – is caused by a blood clot that prevents normal blood flow through the brain and causes neurons to die.
This type accounts for 80% of all strokes. Rapid diagnosis and treatment of acute ischemic strokes is essential to reduce death and disability from stroke.
That’s why learning the FAST acronym is so important:
F = Face: Is one side of the face drooping down.
A = Arm: Can the person raise both arms or is one arm weak?
S = Speech: Is speech slurred or confusing?
T = Time: Time is critical!! Call for urgent medical help immediately!
The other kind of stroke is hemorrhagic, when a blood vessel that carries oxygen and nutrients bursts and spills blood into the brain. When this happens, a portion of the brain becomes deprived of oxygen and will stop functioning. The most common signs of a hemorrhagic stroke are sudden, severe headache with no known cause; partial or total loss of consciousness; vomiting or severe nausea, when combined with other symptoms; and sudden numbness or weakness of the face, arm or leg, especially on one side of the body.
The risk factors for stroke – besides age, gender, genetics and ethnic background – are smoking, hypertension, overweight, diabetes, high cholesterol and lack of exercise.
The main treatments for ischemic stroke are injecting tissue plasminogen activator (tPA), a protein that breaks down blood clots, and performing catheterization to pull the clot out of the blood vessel in the brain or the neck, said Verstandig. “In 2017, we had the largest number of cases of stroke diagnosis and treatment in Israel. We also developed a computer application in which Magen David Adom, the emergency ambulance service, informs us that a stroke victim is on the way. Within 25 minutes of the patient’s arrive, we can perform a CT or MRI scan and bring him to an expert for treatment.”
Mapping of the brain with yellow and red colors can tell radioneurologists how much blood flow in the brain remains and how much tissue has died. “The expert has to build a protocol, decide on the type of examination, give an urgent answer in serious cases when the neurologists are sure and also control amount of radiation. We hold several multidisciplinary meetings every week,” he stated.
Five thousand Israeli women each year are diagnosed with breast cancer, said Dr. David Gechtman, head of diagnostic mammography at SZMC. Mammography and a physical exam are the most basic and safe ways to diagnose it and they identify most of the cancers.
If a breast tumor is nevertheless suspected, MRI is used using a contrast medium, but this can lead to unnecessary biopsies, “so we don’t do an MRI on every woman. There is also 3D ultrasound,” said Gechtman. In younger women, tumors grow faster. It grows more slowly, is smaller and less aggressive in older women.” But he still recommends mammograms for women over 75.
Women should not fear radiation from mammograms, as there is plenty of natural and manmade radiation all around us – from jet travel, radon in the ground, food and drink. “Mammograms emit very little radiation, and they themselves do not cause breast cancer,” he assured the audience.
Summing up, Dr. Yigal Frank – a senior radiologist in the imaging institute, summed up that the radiation their devices emit are the lowest possible and used only when necessary. Contrast media that are injected or swallowed are needed to differentiate between the sick tissue and the rest of the body. “Various diseases can influence the way the tissue is colored, and these differences are vital when diagnosing the condition.”
Although MRIs were introduced after CTs and don’t involve radiation, Frank said that MRIs to not replace CTs and are not the preferred device for all conditions. For example, when a diagnosis is urgently needed or when the bones or lungs have to be scanned, CT is faster and better.
And, he concluded, don’t be surprised when the MRI technician asks you to fill out a questionnaire about metal in your body or your clothing, before the scan. If you suffered a shrapnel wound in the army or had a piece of metal implanted in your body – or if you are wearing something with metal inside – they can be damaged or cause harm.
Source: Israel in the News